In high school during class, I saw one of my classmates fiddling with a small electronic device that resembled a pager. I asked her what it was and she told me it was an insulin pump. I then proceeded to ask her what it was for and she explained that it helped her manage her diabetes. I had no idea what any of that meant until I did my own research. I found that the greatest benefit of using an insulin pump is that it delivers insulin to the body throughout the day; this allows for more accurate and precise dosages of insulin, as well as better control of blood glucose levels. The downside of using an insulin pump is that the pump has to be carried at all times and serves as a constant reminder of the condition.
What is an insulin pump?
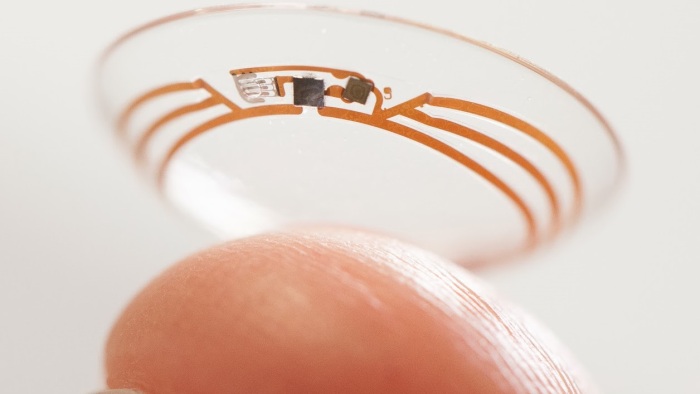
The insulin pump is not a new invention – it has actually been around since the 1970’s – and it continues to be used to effectively manage diabetes. It’s a small electronic device – about the size of a deck of cards – that helps to deliver insulin to a diabetic through the subcutaneous tissue. The pump consists of the main pump unit that holds an insulin reservoir. This is attached to a piece of thin tubing with a needle (cannula) at the end – the infusion set – which is connected into the subcutaneous tissue and held in place with an adhesive patch; it remains connected to the body and controls the amount of insulin delivered by the press of a button.

http://www.diabetes.co.uk
The advantages of using an insulin pump
An insulin pump helps to deliver fast acting insulin throughout the day in order to keep blood glucose levels in a desired range. The rate at which an insulin pump infuses insulin is known as the basal rate and it can be set or changed at any time with the press of a button. Insulin delivery can be programmed to provide different amounts of insulin at different times during the day and night.
When more insulin is needed to address excess carbohydrates from a meal, it’s easily achieved through the push of a button. Insulin pumps can deliver a bolus of insulin in order to cope with high blood glucose levels.
One of the other popular benefits of using an insulin pump is that it decreases the number of injections compared to traditional delivery methods such as through a needle and syringe or an insulin pen. The infusion site is typically changed every two to three days compared to traditional insulin delivery methods that require multiple injections throughout the day.
The use of an insulin pump also helps to reduce the likelihood of hypoglycemia or low blood glucose levels. There is a greater risk of hypoglycemia when taking insulin through injections because larger dosages of insulin need to be taken at a single time. The steady flow of insulin helps to reduce the risk of hypoglycemic episodes which is especially helpful at night during sleep.
Disadvantages of using an insulin pump
Although insulin pumps have become very popular among people with diabetes there are still some drawbacks to to their use. Because the pump is attached to the body, it serves as a constant reminder to wearers and to others of the disease of diabetes.
Using an insulin pump also increases the risk of skin infection at the catheter site which is why the infusion site needs to be changed every two to three days.
Another concern when using a pump is that the cannula can come out from the infusion site which results in no delivery of insulin. This is one of the biggest issues of wearing an insulin pump because if it goes unnoticed for several hours, it can result in diabetic ketoacidosis.
Also not all insurance providers cover the cost of an insulin pump. Insulin pump therapy is more expensive compared to the traditional needle and syringe.
If using a pump is a possible solution for insulin therapy, then a few questions need to be asked:
- Am I okay with having a device attached to me reminding me and everyone else that I have diabetes?
- Am I comfortable with the device and operation of the pump?
- Am I committed to checking my blood glucose levels at least four times throughout the day?
- Am I ready to have a full understanding of insulin, carbohydrate consumption, and activity levels to solve problems related to my blood glucose?
- Do I have a healthcare team that is experience with insulin pumps?